Contents
Introduction
November 5th of this year was the 4th anniversary of having a total knee replacement for my right knee. The surgery was a success and I originally wrote about my journey to it back in August of 2020.
Arthritis being what it is, it seemed only a matter of time when my left knee would start to break down need the same treatment. While I tried to put it off as long as reasonably possible, I've now got the surgery scheduled for March 2025.
I recently met with the orthopedic surgeon who performed the first surgery, Dr. Stefano Bini. X-rays confirmed the severity of the arthritis. But I had a lot of questions about how things have changed in the last four years.
I'll walk you through how I got here and what has changed.
Injections and exercise have bought me time
Interestingly, the first twinge of pain that I got on left knee was shortly before I had my right knee replaced. I was going down a couple of steps in our house and felt a sharp pain. I thought, "Oh no, here we go again." A visit to a local orthopedic surgeon (known in my prior writing as "InjectoDoc") confirmed that I had arthritis in my left knee and offered a cortizone shot to relieve the pain. That worked great.
After I had my right knee replaced, I was back on the tennis court in 6 months and that felt great. I played for about a year when my left knee began to "complain". I went to the same doctor that gave me the cortizone shot and this time, I opted to get a shot of hyaluronic acid along with the cortizone shot. He also prescribed a round of physical therapy. But by the time that I went to the first PT appointment, my knee was feeling great. I went to one session, learned some exercises, and did them at home.
I continued doing those exercises and playing tennis for about a year when the pain returned. I returned to the doctor, got the same shots again. But this time there was no relief. The arthritis had worsened and had gone from being classified as "mild" to "moderate." As of this writing, I have reached the "severe" classification. Lucky me, always achieving!
I continued to do the exercises and played tennis, wearing a knee brace. But after a while, it felt like the pain was hampering my play. So much of my enjoyment on the tennis court comes from the movement. It became rather frustrating letting balls go that I could have made a dash for in the past. And gone were the days where I felt that I was moving gracefully on the court, particularly on my one-handed backhand. It felt like I was dragging my left leg around the court and that made it hard to focus on the ball, throwing off my timing. It simply began to suck.
During this period, I altered my workout routine. It had been kettlebell focused, which I had written about. I changed it to be free weight and machine oriented. The club where we belong had just been acquired and the new owners refurbished the fitness area with new equipment. I found an app, Strong, to track my sets, reps, and weights so that I could get on the "progressive overload" train and add some muscle to my aging frame. I also started doing a 50 minute indoor spin class once a week. So, now I had a routine of Mondays and Fridays doing a full body weight training workout and Wednesdays doing the spin class.
All of this bought me some time, but it seems that my time has run out. On the upside, our spin instructor recently pointed out that leg strength is highly correlated with longevity in men, though I bet it's also true for women. I went home and did some digging and it seems that there is indeed research to support that claim. So, I've got that going for me.
I can only delay this for so long
I was in denial, thinking that I could put off replacing the knee until late 2025. I could still walk for miles without pain. When I had my right knee replaced, I waited until I was limping on every step and could not walk a block without wanting to go back.
But the pain began to show itself in various ways and more frequently. I might be sitting and one false move would cause a sharp pain. When I get into the car to drive, that act of having to shift my weight and bend my left knee at an angle became an affair of managing that angle closely to minimize how much pain the act would cause.
Thankfully, walking remains nearly pain free. We recently returned from a trip to Italy and we were walking close to 20,000 steps per day. At the end of the day, my knee would be a bit swollen, but during the day, I had only small amounts of pain during the walks.
I had been hoping to schedule the surgery for early January to take advantage of the winter, but the surgeon's schedule was full until March. I was a bit disappointed, but I'm glad that I have the extra time to prepare. We had been planning to go to Europe in late May, but we're going to have to reschedule that for the fall as I definitely won't be ready to travel by May.
The important thing for me now is to continue my weight training and spin class so I can be in good shape prior to the surgery. I am hopeful that by doing that, recovery will be a bit easier, and perhaps faster. We'll see.
Let's get into what has changed in the last four years in the realm of knee replacement. And specifically, how my surgeon's approach has changed.
A robot has entered the chat
Among the more recent developments in total knee (and hip) replacement surgery is the use of robots. Note that the robot assists the surgeon, it does not perform any work itself.
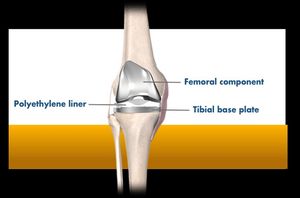
In my right knee replacement, the surgeon used an implant made by the Stryker company. They manufacture a robot they call MAKO.
Recent research indicates that a robot-assisted knee replacement results in "...better short-term clinical efficacy, achieved better alignment planning, and maintains good safety." Additional research indicated that there is a "greater improvement in knee-specific pain but not in function."
In my meeting with the surgeon, when asked about the robotic assist technology, he said that it was an option. He said that in his experience, it provided more accuracy.
How is that accuracy achieved? One new pre-op requirement for a robotic assisted surgery is getting a CT scan of my knee. This allows the MAKO software to create a 3D model of my knee which can be viewed during surgery. There are also a couple of tracker pins that are inserted into my femur and tibia during the surgery to provide inputs to the location of these bones during surgery.
It's really pretty cool technology and I'm up for it. I do have a couple of questions that I'll pose to the surgeon as I make my way to the operating table. Among them are:
- How many robotic assisted surgeries has he performed?
- What does he do if the robot goes down or is not available?
- Has he seen better outcomes with the robotic assist?
These questions came from a set prepared by an orthopedic surgeon that I follow on YouTube. His name is Adam Rosen and his videos are an excellent resource for all things knee replacement. He even has a book, titled "The Knee Book," which I have read and highly recommend if you find yourself in a similar situation.
So that's the one change since my first knee replacement. Let's look at a couple of other changes.
My right knee implant was cemented
Knee implant tecnology has also advanced as have the methods of affixing the implant to the bones. In my right knee replacement, the surgeon used a cemented implant. This means that the implant was glued to the bones using a special cement. The cement they use hardens exceptionally quickly. As a result, the strength of the bond achieved is quite high. In fact, at the time of the implant, this is the strongest that it will ever be as future jarring or other movements can cause loosening of the implant.
A more recent development has been the use of cementless implants. The way these work is that the bone side of the implant has a special textured surface that attempts to mimic the porous nature of the bone. The idea is that the bone will grow into the implant and create a bond that is as strong as the original bone. In this case, the implant-bone attachment is at its weakest at the time of the surgery and gets stronger over time.
This idea about the time of greatest strength of cemented vs. cementless implants is not something that I had thought about. But it makes sense. Here's an excellent 15-minute video by Dr Kevin J. Choo discussing it.
I recall asking my surgeon at the time of my first knee replacement if he was going to use a cementless implant. At the time, he said that he uses cemented implants because he has had good success with them. When I asked him about this for my left knee, he said that he would use a cementless implant.
In my research, cementless implants show good results. But it's important during the first 6 weeks of healing that the implant not be jarred, allowing the bone to grow into the implant.
There are pros and cons to each approach. The use of cementless has historically been for younger patients with younger bones. But the technology has advanced, and there has been research supporting the approach as a viable option for older patients as well. There is some evidence, though not long term, that cementless implants may last longer than cemented implants as cemented implants are more likely to loosen over time.
And when you go cementless, there's another change that typically happens in the procedure.
I won't miss the tourniquet on my thigh
It turns out that using a cemented implant can sometimes dictate the use of a tourniquet on the thigh. I recall reading the operative report from my first surgery and it noting that the tourniquet was on my thigh for about an hour. I had wondered what the upper leg soreness was coming from.
The purpose of using a tourniquet was to create what is known as a "bloodless field," the goal of which is to improve cement penetration and the bone-cement interface. But that purpose has been called into question by some researchers.
The benefit of not using a tourniquet is that it reduces the time of the surgery by a small amount. Questions have also been raised about the need for tourniquets even in cemented implants. In fact, there is research that indicates that using a tourniquet "...decreases the thigh and quadriceps muscle volumes and postoperatively delays the recovery of knee function."
Perhaps all this is too much information. But I had the itch to get it down on "paper" and share it. I hope that it's helpful to someone.
How am I preparing?
So, now I'm in the preparation phase. Today is December 1st. I have a little more than 3 months until the surgery. I will continue to maintain my exercise regimen in the hopes of having the strongest legs (and other body parts) that I can have prior to the surgery. Even if the recovery is not any easier or quicker than my first surgery, I will be able to more easily return to a solid fitness level after the surgery.
Conclusion
If you've gotten this far, thank you.
A lot has changed in the knee replacement technology field in the last four years and much of it is for the good. I am glad that I have a surgeon that keeps current with the advances in knowledge of this rather amazing procedure. I am also glad that I have a surgeon that is willing to answer my questions and is willing to listen to my concerns. If you live in the San Francisco Bay area and need a knee or hip replacement, I can definitely recommend my surgeon, Dr. Stefano Bini, at UCSF.
There is a part of me that is not looking forward to the surgery...at all. I have less-than-fond memories of the first surgery and the recovery. It was incredibly difficult to get a good night's sleep for the first six weeks. That, and other minor annoyances, made the recovery a bit of a slog. I recall becoming frustrated at around month two with the exercises and the pain that they brought. But I stuck with it and I'm glad that I did and the outcome has been very good. It's just not a lot of fun.
While I won't be able to exercise during the recovery process as I do now, I will have plenty of reading time as well as time to continue writing here and maintaining the 11ty Bundle website.
Previous post: Happy Thanksgiving 2024
Next post (in time): Going all in with 'native' markdown