NOTE: This piece was originally posted on Medium, on August 31st, 2020. I underwent total knee replacement surgery on November 5, 2020, smack in the middle of the pandemic. The good news is that the replacement went very well and now, 3 years later, I'm very glad I did it.
Contents
Introduction
I turned 65 this month. My mind doesn’t think so, but my body knows it and it’s been trying to tell me. It’s a knee thing. It hurts and it’s been hurting for the last few years. The pain has made it less than pleasant to walk a single block. It’s keeping me off the tennis court. And I’d like some relief. Do I need a knee replacement or is there another way?
I’ve been playing tennis, on and off since I was 19. I picked it up during college in Florida. It was the early ’70s and there was a major explosion of the sport and south Florida was a hot spot. I played a little handball in college too. It was great for my tennis; you really had to be able to react quickly, move fast, and stay low. And I ran a little bit during my post-college days, doing the occasional 10K and a single half-marathon. That half-marathon was long enough for me.
Up until I hit 60, when others would start to complain about their knees, I would brag that I hadn’t had any trouble with my knees. My game relied on my movement...not that I did a lot of winning. I’m not an offensive player, more of a defensive — get the ball back at any cost — player, trying to frustrate my opponents. I loved just getting to the ball and hitting it, trying to be as smooth as possible.
Well, a few years ago, one of those knees that I’d been bragging about decided to serve notice that its pain-free state was ending.
Earlier this year, things came to a head where I was unable to walk very far without each step announcing itself with a cringe. But let me back up a few steps and review the early signs and my attempts with various interventions.
Is there a doctor in the house?
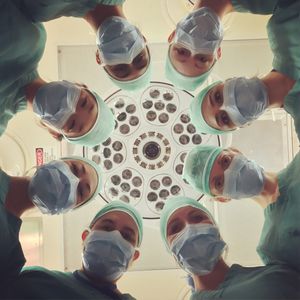
Photo by National Cancer Institute
Several years ago, when we lived in Bellevue, Washington, I decided to see a doctor to get a professional take on what was going on. X-rays revealed osteoarthritis of both knees, with the right knee winning the degeneration race. From the x-ray report:
Moderate medial compartment right knee and mild medial compartment left knee joint space narrowing is present.
The doc said to try physical therapy. I did, deploying ice and Advil as needed and doing some specific exercises to strengthen the muscles around the knee. It was working reasonably well. I was able to keep playing.
Last year, after moving back to California (we’ve moved a lot), my wife was getting a PRP (Platelet Rich Plasma) injection for her hip. I asked the doctor if it was suitable for knees. He suggested that I first try a cortisone injection, which he offered to do on the spot. I said what the heck. It had no effect; the pain persisted. Several months later, I went to see him again. This time, he suggested that I try a PRP injection…what the heck. It had no effect; the pain persisted.
This year, after the arrival of COVID-19, I’ve been reluctant to seek additional medical advice. Yet an unfortunate mishap, going down 2 steps and torquing my left knee, resulted in excruciating pain. And I thought I had a bad right knee. Later that evening, I had one of my occasional episodes of atrial fibrillation (a fast and irregular heartbeat). I have about 6 to 8 of these a year. I carry a pill with me that usually gets my heart back to a normal rhythm within an hour or so. Not so, this time. Shortening the story, my wife took me to the ER where they got my heart back to normal (thank you, ER docs). I suspect it was triggered by the stress of the knee injury.
Back to my knee. I called to schedule a visit with the doctor that had given the 2 injections (soon to be known as InjectoDoc). He took some new x-rays and said that the right knee needed to be replaced as it was bone-on-bone…the cartilage was gone. He gave me a cortisone injection in my newly injured left knee. Fortunately, I had a positive response and the pain was dramatically reduced. He also ordered an MRI of the left knee to see the extent of the injury and if it might need a surgical repair.
At a follow-up appointment, the left knee felt much better. The MRI showed some minor meniscus tears, but nothing that would require surgery. I asked about options for my right knee, short of a full replacement. He offered 2 types of injections. One is called viscosupplementation. From that article:
Viscosupplementation is a procedure in which a thick fluid called hyaluronate is injected into the knee joint. There are no cures for osteoarthritis, so viscosupplementation will not cure osteoarthritis of the knee. However, it is thought that hyaluronate will improve the lubricating properties of the synovial fluid, reduce the pain from osteoarthritis of the knee, improve mobility, and provide a higher and more comfortable level of activity.
The second one is called Lipogems, where they take some fat from one part of your body, they break it down and then re-inject it into the knee.
If I’m going to try another injection, how best to decide on which of these to choose? Most of the orthopedic doctors that I’ve looked at online offer viscosupplementation, but few seem to offer Lipogems. The breadth of availability of the visco-stuff would be one factor in my choice. And since the description of the visco-stuff said “it is thought that hyaluronate (aka, visco-stuff)…will improve…,” I decided to go with the visco-stuff.
That visit with InjectoDoc was in July. I told him that I’d like to try the visco-stuff. He said that if I have private insurance, they would not likely cover it. So I scheduled it for late August; by then I will have arrived to the wonderful world of Medicare, which does cover it. The particular brand of visco-stuff that I’d be getting is called Synvisc-One.
Is this the doctor I should be seeing?
InjectoDoc (also, Joe Jackson)
I was starting to become concerned that InjectoDoc might not be the right guy for my long term knee care. I was relying on the fact that he was conveniently located. That, and a yoga instructor suggested him to my wife to help diagnose her hip (I kid you not).
The other worry I had was that the health system portal that shows test results had no written radiology reports from the x-rays or the MRI that had been done. I wanted to know more.
What do the clinicians who do research say?
Since we live only an hour north of San Francisco, I thought it might be best to look for an orthopedic surgeon at the UCSF Department of Orthopedic Surgery, a teaching hospital. My cardiologist is a UCSF doc and he’s been great.
So I started looking at the bios of all of the orthopedic surgeons at UCSF that work on knees. I located one doctor that caught my eye. What got me interested was this statement in his bio:
…will continue to focus on total hip replacement through both anterior and posterior approaches, and total knee replacement using a novel anatomic alignment technique (“kinematic” knee alignment).
Kinematic knee alignment? What the heck is that? So I dug and I dug and I dug. I learned that there are multiple approaches to aligning a knee replacement, one of which is kinematic alignment (3D) and the others (2D, mostly referred to as mechanical alignment). Here’s a description of the differences:
Kinematic alignment considers the 3D alignment of the components with respect to the knee instead of the 2D alignment of the components with respect to the center of the femoral head and ankle. The intent of kinematic alignment is the restoration of the normal 3D orientation of the three axes that describe normal knee kinematics.
From the articles I’ve read, when it comes to pain reduction and knee function, approximately 20% of patients undergoing knee replacement using the 2D alignment technique are dissatisfied with the results. Kinematic alignment is aimed at improving those results, and there seems to be evidence supporting this.
So I made an appointment to see him and scheduled it before my date with InjectoDoc. He’s a surgeon and knee replacements are one of his specialties. Of course, he said that I needed a knee replacement. His story to me went something like this.

Your roof is leaking
“Your roof is leaking. You can wait, but your roof will still be leaking. At some point, you’ll need to fix it.”
I asked him about the various injections, noting that cortisone and PRP did nothing for my right knee. I asked about visco-stuff and fat. He said that they didn’t work. I asked about CBD cream. He said that he has no problem leveraging the placebo effect. I chuckled. He did say, seriously, that it could reduce some of the pain pathways, taking the edge off and providing a level of calm.
I noted that I was concerned about being in the hospital during COVID-time and that I’d feel better doing a replacement after the start of the new year. He understood, but noted that I’d be going home the same day. I said that I’d consider what he’d said and would let them know. They provided some home exercises to do in preparation.

That’s my right knee…on the left.
The next day, I was notified that the radiology report was available. Here’s a portion:
Severe joint space narrowing of the right medial femorotibial compartment with bone-on-bone articulation. Mild joint space narrowing of the left lateral greater than medial femorotibial joint spaces.
Shit! I’ve gone from moderate to severe on the right knee. Silver lining…the left remains mild.
I copped some CBD cream at $35/oz. I tried it for a few days. It didn’t seem to do much other than provide my wife and me with something to crack jokes about.
Have any of these injections been proven to work?
With all the noise coming out from all corners of the propaganda-sphere about therapeutics for COVID-19 and the lack of evidence for some of them, I started to wonder about all of these knee injections. So I started digging into the research and the recommendations from the professional organizations, like the American Academy of Orthopaedic Surgeons.
Not surprisingly, they have a set of Clinical Practice Guidelines for the treatment of osteoarthritis of the knee (here’s the summary). These are “evidence-based recommendations,” all 1,234 pages of them.
The recommendations section starts out with this:
This summary of the AAOS clinical practice guideline, “Treatment of Osteoarthritis of the Knee” contains a list of the evidence based treatment recommendations and includes only less invasive alternatives to knee replacement.
This is exactly what I was looking for. This is where I would find all the answers.
These guidelines are “…based on a systematic review of published studies examining the non-arthroplasty treatment of knee osteoarthritis in adults.”
So what do they say about cortisone, platelet rich plasma, viscosupplementation, and fat? Let’s take a look.
Corticosteroids, AKA cortisone. “We are unable to recommend for or against the use of intraarticular (IA) corticosteroids for patients with symptomatic osteoarthritis of the knee.”
Platelet Rich Plasma (PRP). “We are unable to recommend for or against growth factor injections and/or platelet rich plasma for patients with symptomatic osteoarthritis of the knee.”
Hyaluronic Acid, AKA visco-stuff. “We cannot recommend using hyaluronic acid for patients with symptomatic osteoarthritis of the knee.”
Lipogems, AKA fat. The guidelines did not weigh in on the fat injections, placing a heavy burden of proof on those advocating them (puns intended).
The guidelines provide “Implications” for each of these types of recommendations.
In the case of the inconclusive recommendations, where they are “unable to recommend for or against,” they say:
Practitioners should feel little constraint in following a recommendation labeled as Inconclusive, exercise clinical judgment, and be alert for emerging evidence that clarifies or helps to determine the balance between benefits and potential harm. Patient preference should have a substantial influencing role.
In the case of the strong recommendation, where they “cannot recommend using,” they say:
Practitioners should follow a Strong recommendation unless a clear and compelling rationale for an alternative approach is present.
The cortisone had no effect on my knee pain, the PRP had no effect on my knee pain, yet my “patient preference,” seeking relief, had a “substantial influencing role” in their use. And the practitioner that I had chosen “felt little constraint.”
Ah, but visco-stuff, the guidelines can’t recommend its use, “unless a clear and compelling rationale for an alternative approach is present…” whatever that means.
To inject or not to inject?

Now I was faced with whether or not to keep my appointment with InjectoDoc to get a visco-stuff injection. Perhaps it could buy me a bit more time before a knee replacement.
My brother and cousin both told me that visco-stuff worked for them. That would be my “clear and compelling rationale.”
Once again, I decided what the heck. Let me see if I can at attempt some interim pain reduction and be able to take some longer walks before getting a knee replacement.
InectoDoc said that it can take as long as 6 weeks for the visco-stuff to take full effect. That was 10 days ago…no pain relief as of yet.
As I was drafting this piece, my wife called over from the kitchen and asks if I’d seen the article in that day’s NY Times. It was about growing knee cartilage in mice. I think she’s joking, but she’s not. It’s titled Cartilage Is Grown in the Arthritic Joints of Mice. Here’s the lede:
The painful knees and hips experienced by so many people with osteoarthritis result from a loss of cartilage, which serves as a sort of cushioning in the joints. It had long been thought that cartilage, once gone, cannot grow back.
It goes on to talk about the approach taken by the Stanford researchers, the injections involved, and how much work remains. One doctor, not involved in the research “…worries that orthopedists may not wait for rigorous studies…Faced with patients with aching knees, orthopedists may be tempted to say ‘Let’s try this, you don’t have much to lose.’ That’s the problem with a lot of things in orthopedics. There’s typically widespread adoption before there is evidence.”
That’s the problem with a lot of things in orthopedics. There’s typically widespread adoption before there is evidence.”
And bam! — that “widespread adoption” is the rub, and I realized that I’ve become a participant in it. Even though most of the treatments I’ve tried rely on inconclusive evidence, my doctors are hinting that I don’t have much to lose, and I’m so fed up with my knee that I have to do something about it. Widespread adoption gets halfway around the world while evidence is still putting its shoes on.
The big picture takeaway here, however, is that the science of physiology has a long way to go. An MRI or an x-ray can’t yet point to exactly which treatment should be applied. It’s a doctor-patient engagement crap shoot. What works for some people, won’t work for others and they just can’t reliably tell which treatment will work for which patient.
I’ll end with a note that one of the “strong” recommendations in the clinical practice guidelines says:
We recommend that patients with symptomatic osteoarthritis of the knee participate in self-management programs, strengthening, low-impact aerobic exercises, and neuromuscular education; and engage in physical activity consistent with national guidelines.
So for now, I’ll work on doing the exercises that will strengthen my legs and keeping my weight under control so that I’m ready for that inevitable knee replacement.
Previous post: I left Twitter
Next post (in time): Learning to play the piano
